141 Things to Know about IBS: The Ultimate Guide to Understand, Manage, and Prevent Flare Ups Long Term
40-minute read
Irritable Bowel Syndrome, or IBS, is more common than you may think, affecting between 25 and 45 million people in the United States.
It’s a chronic condition that affects the way the GI system works, with some describing IBS as a brain-gut disorder. While the condition is not life-threatening, IBS can have a significant impact on the quality of life and may cause people to miss a substantial amount of workdays.
Whether you’ve been wondering if you have IBS or have been trying to manage it with the low FODMAP diet for years, this guide is for you.
It covers everything you need to know about what IBS feels like, what foods trigger a flareup, how it’s diagnosed, and most importantly the latest research on how to manage it effectively to improve quality of life once and for all - for yourself or for someone in your life with IBS.
Jump to the section below you’re most interested in or signup to receive a To-Do Checklist in your email inbox
- Essential questions to understand IBS
- Symptoms of and risk factors for IBS
- Women and IBS
- Complications of IBS
- Actionable steps to prevent and manage IBS
- Patient advocacy and community support groups
- Useful Apps
- IBS in numbers
- Latest research
- Dating and relationships
- Work, school, and travel
- Books
- Podcasts
- Documentaries and videos to watch
- IBS trends around the world
- In a nutshell
Essential Questions to Understand IBS
- What is IBS?
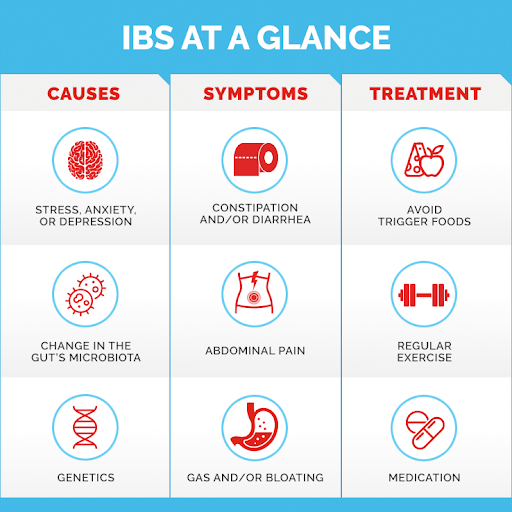
IBS stands for Irritable Bowel Syndrome and is a chronic, functional disorder where the gut and the brain are not working together as they should (known as the gut-brain connection through the vagus nerve). It can show a wide variety of symptoms from one person to the next. Typically though, the key symptoms of IBS show up as a change in bowel habits (constipation or diarrhea), bloating and intense abdominal pain, where you have more than one symptom per week for at least three months. IBS is not IBD (Irritable Bowel Disease), and as a result does not inflame the GI tract or do permanent damage to it. Rather, the major effect of IBS as with many chronic conditions is quality of life can be significantly impaired if not managed properly.
- How many kinds of IBS are there?
There are 3 kinds.
- IBS-D: diarrhea type (post-infectious and non post-infectious)
- IBS-C: constipation type
- IBS-M: mixed type
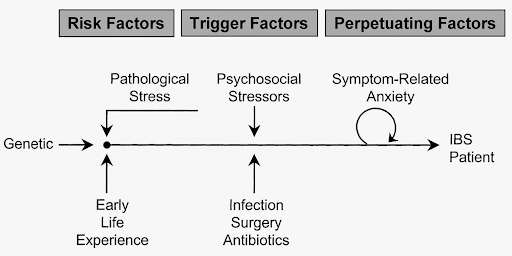
- What causes IBS?
While the root of some IBS cases are food poisoning, small intestinal bacterial overgrowth (SIBO), or hormonal, others are still unknown. Several factors can amplify symptoms such as stress, being a woman, oversensitive nerves, or lifestyle habits. If you have a family history of IBS, then you may be more likely to develop it.
Some lifestyle habits may also contribute to the condition and exacerbate symptoms.
- How do you test for IBS?
For IBS-D and IBS-M, a blood test has been developed by Dr. Pimentel that measures elevated antibodies to reach a diagnosis. In many cases, IBS diarrhea and mixed are developed after food poisoning, even years afterward.
In 2017, a Mayo Clinic study found that IBS develops for 1 in 9 people after having food poisoning, especially if antibiotics were used to treat it. In fact, having food poisoning puts you at a 4x higher risk to develop IBS outside other risk factors. Food poisoning alters the microbiome and leaves behind antibodies that can be traced in the blood. The IBS-Smart Blood Test developed by Dr. Pimentel confirms that the source of IBS-D and IBS-M are microbiome based and not caused by stress, lifestyle, psychological trauma, and other risk factors like age or gender.
For IBS-C and those who score negative on the blood test but IBS is still suspected, a doctor will diagnose the condition by taking your medical history and, if necessary, carrying out an examination. To reach a diagnosis, you must fit the Rome IV criteria of having more than one symptom per week for at least three months, a change in bowel habits (constipation or diarrhea), and change in stool consistency.
Your doctor may also feel it’s necessary to carry out more comprehensive tests. This may mean:
- A colonoscopy to rule out other conditions that may cause similar symptoms, such as colon cancer or celiac disease.
- X-rays.
- C-scan.
As well as imaging tests, your doctor may order some laboratory tests, such as:
- Lactose intolerance tests.
- Bacterial breath tests (such as the SIBO test - one of the most advanced, at-home breath tests from Dr. Nirala Jacobi at the Biome Clinic in Australia).
- Upper endoscopy tests.
- Stool tests.
- Food sensitivity tests (such as the York test that covers over 200 ingredients).
- Blood tests (to rule out an underlying infection).
For people with suspected IBS-D and IBS-M who have not had food poisoning in their lives or show negative on the blood test, you may still have IBS caused by an underlying condition. Digging deeper with your healthcare provider should be a priority in order to cure or manage the condition causing IBS.
It is important to note that IBS can occur alongside other serious conditions, so if you have additional symptoms not explained by IBS
- Which foods trigger IBS?
Although the foods you eat don’t lead to the development of IBS, some may worsen the symptoms by exacerbating distention and bloating. The food triggers may differ from person to person, so it’s often suggested that you keep a food diary to see if you spot any patterns and share it with your doctor.
In your diary, you can record what you’ve eaten, any symptoms you may have, and any symptoms you experience after eating certain foods.
The most common IBS symptom food triggers are:
- dairy
- caffeine
- alcohol
- carbonated drinks
- chocolate
- cruciferous vegetables
- gluten (for some)
- and FODMAPs
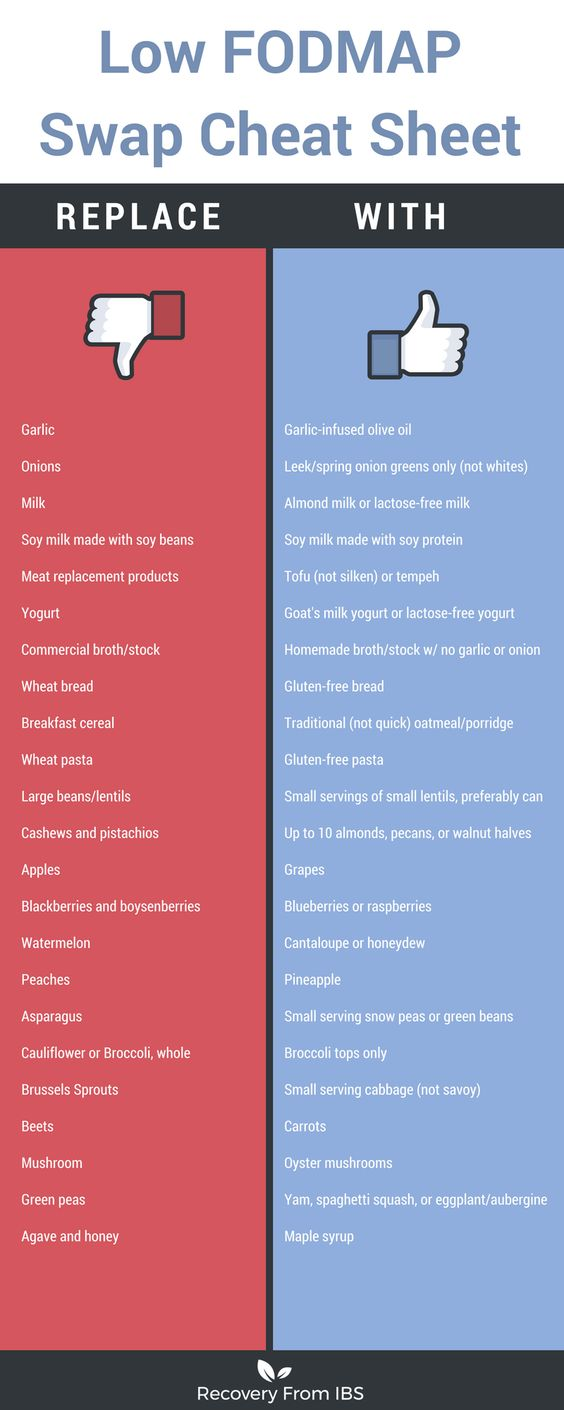
Studies with IBS patients have found that reducing your FODMAP intake can help to improve IBS symptoms on a short-term basis under the direction of your doctor as it is not intended for longer than 6-8 weeks.
While you should cut out foods you find to be triggering, it’s also important that you maintain a balanced diet with a good mix of vitamins and minerals for your overall health. It is important to work with your doctor not only to eliminate foods but build them back in when possible, or finding a nutritionally appropriate alternative because many of the most common triggering foods for IBS (garlic, onion, prebiotics in vegetables) are vital for microbiome health. If cut out for too long, people with IBS become susceptible to secondary conditions like small intestinal bacterial overgrowth (SIBO), leaky gut, and more.
- What are FODMAPS?
FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols. FODMAPs are carbohydrate-based foods that aren’t always properly absorbed in the small intestines of people with IBS. They not only increase the amount of fluid in your bowels, but can also cause more gas, bloating, and reduce digestion speed. This can lead to pain and diarrhea. In severe cases, your doctor may recommend following a low FODMAP elimination and reintroduction diet for immediate IBS symptom relief.
It is very important to note the low FODMAP diet should be followed under the direction of your healthcare provider, for no more than 6-8 weeks.
The low FODMAP diet was designed as a “band-aid” for temporary relief of symptoms, but it was not designed to heal the gut. The diet eliminates all too important prebiotic and fiber-rich foods such as onions, garlic, and legumes, and reduces microbiome diversity. Fiber is critical to decrease bloating, pain, and other symptoms of IBS, though it is important to work them in slowly.
- How do you treat IBS?
There is no cure for IBS right now, but there are clinically proven ways of managing the condition as if it were in remission. This may involve medication or lifestyle changes. As you’ll read later, stress is a major contributor to IBS symptoms, so your doctor may suggest introducing a relaxation program to retrain the communication between your gut and your brain. Some additional lifestyle changes could include:
- Getting more exercise.
- Getting more sleep.
- Giving up tobacco and alcohol.
- Following a low fat, high-fiber diet.
If these simple lifestyle changes aren’t enough, your doctor might suggest you try medications. The medicine you’re prescribed will vary depending on your type, but here’s a list of the most common ones:
For IBS-D, the most commonly prescribed medications include:
- Lotronex for female sufferers of IBS.
- Xifaxan.
- Loperamide.
- Eluxadoline for IBS-D types.
Your doctor may also suggest additional fiber supplements or laxatives.
For IBS-C types, your doctor may prescribe:
For stomach pains, you may find a natural approach like peppermint oil useful. If the pain is more severe, your doctor may prescribe antispasmodics or antidepressants.
- What is the microbiome?
The microbiome is the community of bacteria, fungi, and other viruses that live in and on the human body. There are 100 trillion bacteria cells (10 times more than human cells) and they play critical roles in maintaining human body functions, preventing disease, and digestion among others. Often referred to as the “the second brain”, the majority of the microbiome resides in the gut. When the microbiome diversity is compromised, it is less able to perform body functions, prevent disease, and digest properly. Unsurprisingly, it was found in a recent study that symptom severity in IBS is negatively associated with microbial diversity. Research is still being conducted about what exact strains of bacteria are related to IBS, but we do know that managing IBS starts with rebuilding the microbiome’s diversity.
- What does IBS pain feel like?
Most people with IBS experience abdominal pain and describe it as very sharp cramps located in the lower portion of the gut and it is often resolved after a bowel movement. Some feel it as a generalized ache with periods of cramps.
- Is Irritable Bowel Syndrome the same as Inflammatory Bowel Disease (IBD)?
No. IBS is a functional disorder while IBD is a structural disorder, meaning there is physical damage done to the bowel as a result of inflammation. There are a lot of myths out there about IBS, so let’s clear them up. What IBS is not:
- Is not caused by your diet
- Is not caused by stress
- Is not a risk for cancer
- Is not a risk for colitis
- Does not cause intestinal inflammation (as opposed to IBD)
- Does not cause malnutrition
- Does not get worse with age, and
- Does not shorten life span
- What doctor cares for people with IBS?
A gastroenterologist is a specialist in gut conditions and will be important in working with you to define your treatment plan. Since IBS is amplified by lifestyle factors (diet, stress, exercise), your care team may also include a psychologist to help with stress management and a personal trainer or fitness coach.
Symptoms of and Risk Factors for IBS
- What are the symptoms of IBS?
Symptoms of IBS can exhibit differently for everybody; however, according to the Rome IV diagnostic criteria for IBS, you must be experiencing recurrent abdominal pain or discomfort for the last three months in addition to at least 2 other gastrointestinal changes relating to frequency or stool appearance.
The most common are:
- Constipation
- Diarrhea
- Abdominal cramps
- Excessive wind
- Increased urgency and frequency
- Sense of incomplete defecation
- Heartburn or acid reflux
- Mucus on the stool
- Intermittent upper abdominal discomfort or pain (dyspepsia)
- Nausea
- Bloating
- Distension
- Anxiety
- Depression
- Headache
- Sexual dysfunction
- Pain during intercourse
- Fatigue
- Lower back pain
- Muscle pain
- Restless sleeping
- Constipation is when you have three or fewer bowel movements a week.
It happens when stool remains in the colon for too long and too much water is absorbed, causing stool to become lumpy or hard and straining to have bowel movements. Constipation can be caused by a number of things from medication depression or heart disease (and more), to a low fiber diet or low exercise lifestyle, communication between the gut and brain, and bacterial or hormonal problems which often start in the microbiome. Constipation can be reversed by correcting the underlying problem with your doctor, slowly increasing fiber intake, and increasing physical activity.
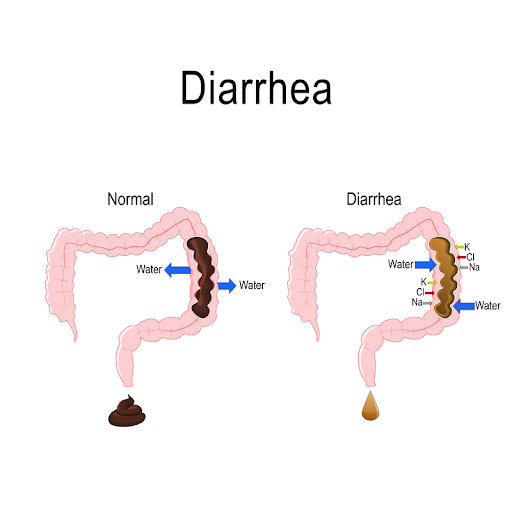
- Diarrhea is when stool has too much water in the colon.
When stool moves too quickly through the colon and produces loose, watery stools, three or more times a day you have diarrhea. It can be triggered by a number of foods and beverages (alcohol, drinks with caffeine like coffee and soda, carbonated drinks, chocolate, artificial sweeteners, fried food, milk products, and legumes in certain quantities), as well as the gut-brain connection. When your nervous system - found in the intestinal walls - communicates with the brain and tells your muscles to squeeze too hard, the result is moving the stol too quickly through the colon. Avoiding trigger foods, increasing soluble fiber slowly, and retraining your gut to calm down through clinically directed hypnotherapy can help reduce diarrhea.
- Abdominal cramps are the number 1 symptom affecting quality of life.
For people who struggle with managing their IBS, abdominal cramps are a result of bacteria fermenting in the colon - either too much or in the wrong place. Eating high FODMAP foods can cause abdominal cramps because they draw additional water into the gut. Bacteria in the gut may then cause them to ferment and increase intestinal gas, expand inside the colon and cause sharp lower abdominal cramps. Avoiding foods like onions, avocados, lentils, garlic, beans, almonds, and cashews for a little while is the start of an IBS healing protocol.
- Excessive and smelly wind should not be ignored because it’s a clue.
Although all subtypes of IBS have excessive wind as a symptom due to increased fermentation of bacteria in the colon more than in healthy bodies, constipation dominant subtypes have been linked to an increase of methanogens in the gut (or methane). Methanogens have long been proven to slow motility.
- No shame in being prepared for increased bowel urgency and frequency.
Slightly more often associated with IBS-diarrhea, increased urgency to have a bowel movement is one of the main symptoms of the condition, and as such can greatly impact quality of life - so it’s important to fend off anxiety about it by being prepared with a plan. Many people find wearing adult incontinence underwear during a flare-up to be a good backup plan, though communicating to those who may need to know about a medical condition’s accommodations (like flexibility to use the restroom, or working from home) are also important.
Find resources for a doctor’s note for your employer, a medical bathroom card and more in the Work, school, and travel with IBS(#Work--school--and-travel -with-ibs) section and public restrooms in the
- Sense of incomplete defecation does not mean strain, please.
Because the nerves in the gut are hypersensitive in people with IBS, it is often difficult to feel a sense of completeness after defecating, and is one reason why when combined with a microbiome healing dietary protocol, gut-brain relaxing therapies can assist in reducing the symptoms of IBS like incompleteness. Straining during a bowel movement though should never be done as it can lead to more complications like hemorrhoids and bleeding, or more severe such as a rectal prolapse.
- Heartburn or acid reflux, also known as GERD (Gastroesophageal reflux disease) is an early sign of IBS.
GERD is a digestive disorder where the contents of the stomach reverse back up into the esophagus, and occurs when that sphincter is weak or relaxes inappropriately. It can in most cases be relieved through dietary and lifestyle changes by reducing acid. Smoking weakens the sphincter, as does the following foods: chocolate, peppermint, fatty foods, caffeine, alcoholic beverages, citrus fruits and juices, tomato products, and pepper. Avoiding those and eating smaller meals at least 2-3 hours before bed will help reduce acid reflux naturally.
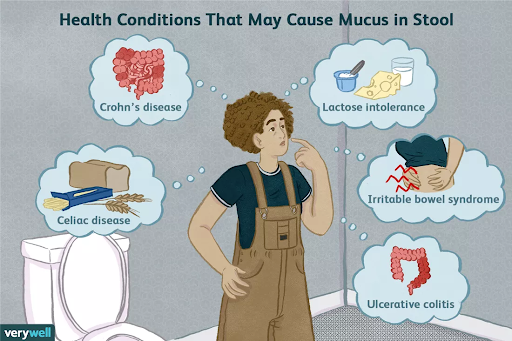
- Pay attention to visible mucus on the stool.
It is a normal function of the mucous membrane of the large intestine to help pass stool through the colon; however when you can see it on stool there is usually a bacterial infection or sign of fissures. Dehydration (often associated with diarrhea), constipation, and lactose intolerance can cause mucus from the colon to leave the body. Visible mucus on the stool is important to notice because the underlying causes can be serious and may require tests. Whether it is caused by food poisoning, IBS or Crohns, an obstruction, or food allergies, it must be treated because it can cause inflammation that breaks down the mucous membrane leaving the body more open to infection.
- Intermittent upper abdominal discomfort or pain (functional dyspepsia).
Another functional disorder, dyspepsia, often occurs alongside IBS. Patients of both conditions are similar in that symptoms are typically chronic in nature, have a genetic predisposition, history of a prior infection, may wax and wane, are aggravated by psychosocial stressors, and are often worsened by meals. Researchers have taken notice and thus far maintain they are different disorders though studying each may provide insights into how to treat the other, “These similarities raise the issue of whether IBS and dyspepsia are just different manifestations of the same disorder or whether they represent distinct clinical entities. Elucidating this clinical dilemma is important because it may improve our ability to diagnose and treat these common disorders.”
- Nausea can be associated with IBS or another condition.
Despite nausea occurring in 27-38% of people with IBS, there is not a great deal of science backing up why. Current theories suggest stronger than normal intestinal contractions during digestion, acute gastrointestinal disease, abnormal signals between your intestines and brain, some foods and medications can cause nausea (listed below). Keeping track of triggers through an app can help determine if you experience a change in symptoms potentially unrelated to IBS, such as:
- antibiotics
- antidepressants
- aspirin
- narcotics
- nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- birth control pills
If nausea continues, your doctor may prescribe anti-nausea tablets like Compazine and Compro to help relieve these symptoms.
- Distension, what it is and what it isn’t.
According to the Rome Foundation which led the research in determining the Rome IV criteria for diagnosing IBS, distension is not caused by an accumulation of excess gas in the abdomen, but by swelling of the abdomen. “Instead the distension is called a visceral (gut) somatic (abdominal muscles) reflex that is triggered by the bloating sensation via the dysregulation of the brain-gut axis.” Distension is what so many IBS sufferers refer to when they “look five months pregnant” and have to loosen their clothes. Dr. Drossman of the Rome Foundation explains the difference between distention and bloating in a video Facebook Q&A here.
- Bloating is the feeling of exceptional fullness especially after meals.
Bloating is a result of the distension of the bowel. The most common culprits are dairy products containing lactose and cruciferous vegetables like broccoli and cauliflower. Regular exercise to improve motility and avoid constipation (which often makes bloating worse), beginning an IBS protocol with a trained gastroenterologist to slowly increase fiber and repair the microbiome while avoiding trigger foods, drinking water and eating smaller meals can help reduce bloating.
- Headaches affect 23-53% of people with IBS, a 2005 study published in the Polish Journal of Neurology and Neurosurgery found.
Researchers don’t fully know yet why this is the case, but some initial theories posit that migraines are caused by a lack of serotonin (95% of which is produced in the gut), or that stress in the gut is impacting the head thanks to the bidirectional gut-brain axis. Another theory comes from the researchers in the Current Pain and Headache Reports traced the link to a genetically sensitive nervous system that turns overly vigilant, which over time can lead to chronic pain such as IBS and migraine headaches.
- Decreased sexual drive is the most prevalent gynecological issue associated with IBS.
In one study, 43% of people with IBS reported sexual dysfunction symptoms, including pain during intercourse, as opposed to people without IBS. Research is still out on why, however gynecological issues seem to affect men and women of various ages the same. Due to more regular hormonal changes, women also report more painful menstruation (dysmenorrhea) and premenstrual syndrome (PMS) compared to those without IBS.
- Fatigue commonly coexists with IBS.
Because chronic fatigue is it’s own condition that is not well understood either, it is hard for the medical community to know how to treat them both or together. One study looking at Chronic Fatigue Syndrome (CFS) and the overlap with IBS found nearly half of participants with CFS also had IBS. More research is needed but initial theories suspect since they share many of the same potential causes (infection, immune problems, heightened pain perception, and more), they suspect a link in terms of similar treatments.
- Lower back pain, especially at night.
Doctors don’t know yet why people with IBS often list lower back pain as a symptom accompanying IBS, but current theories are the pain is “referred” - or felt somewhere other that where it originates. Cramping in the stomach for example can sometimes show up as lower back pain as well. Yoga, massage therapy, meditation, and acupuncture can help. Some probiotics have shown early signs of reducing IBS symptom pain, such as Lactobacillus strains (such as L. acidophilus, L. plantarum, and L. casei) and Bifidobacterium strains (such as B. infantis, B. longum, and B. bifidum) for diarrhea, or B. infantis 35624, L. rhamnosusGG, S. boulardii for constipation.
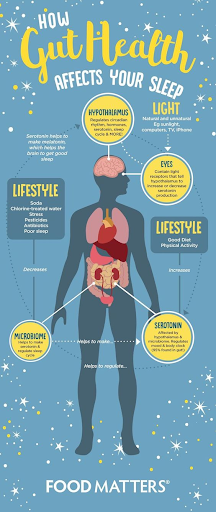
- Restless sleeping is a symptom and risk factor for IBS.
Sleeping problems are common in people with gastrointestinal disorders and are a risk factor for IBS.
- Anxiety and depression are common psychological symptoms in 50% of people with IBS.
Scientists explored the overlap in a 2016 study that tracked 1,900 Australians over time and found that subjects who had IBS-like gut symptoms with no mood problems at the beginning of the study showed higher levels of anxiety and depression one year later. Additionally, two thirds had seen gut symptoms show up before the psychological symptoms, making it unlikely that the brain causes GI symptoms. Even more, in a 2012 study researchers found specific microbiota patterns (called ‘signatures’) determined motility speed and correlated with levels of depression.
Currently, scientists’ working theory is that the bacteria in the gut in IBS is a factor that either initiates psychological symptoms or contributes to them.
- Can symptoms change over time?
Yes, people with IBS can experience a change from having constipation to diarrhea, or both in the same flare-up, or they can change over a longer period of time.
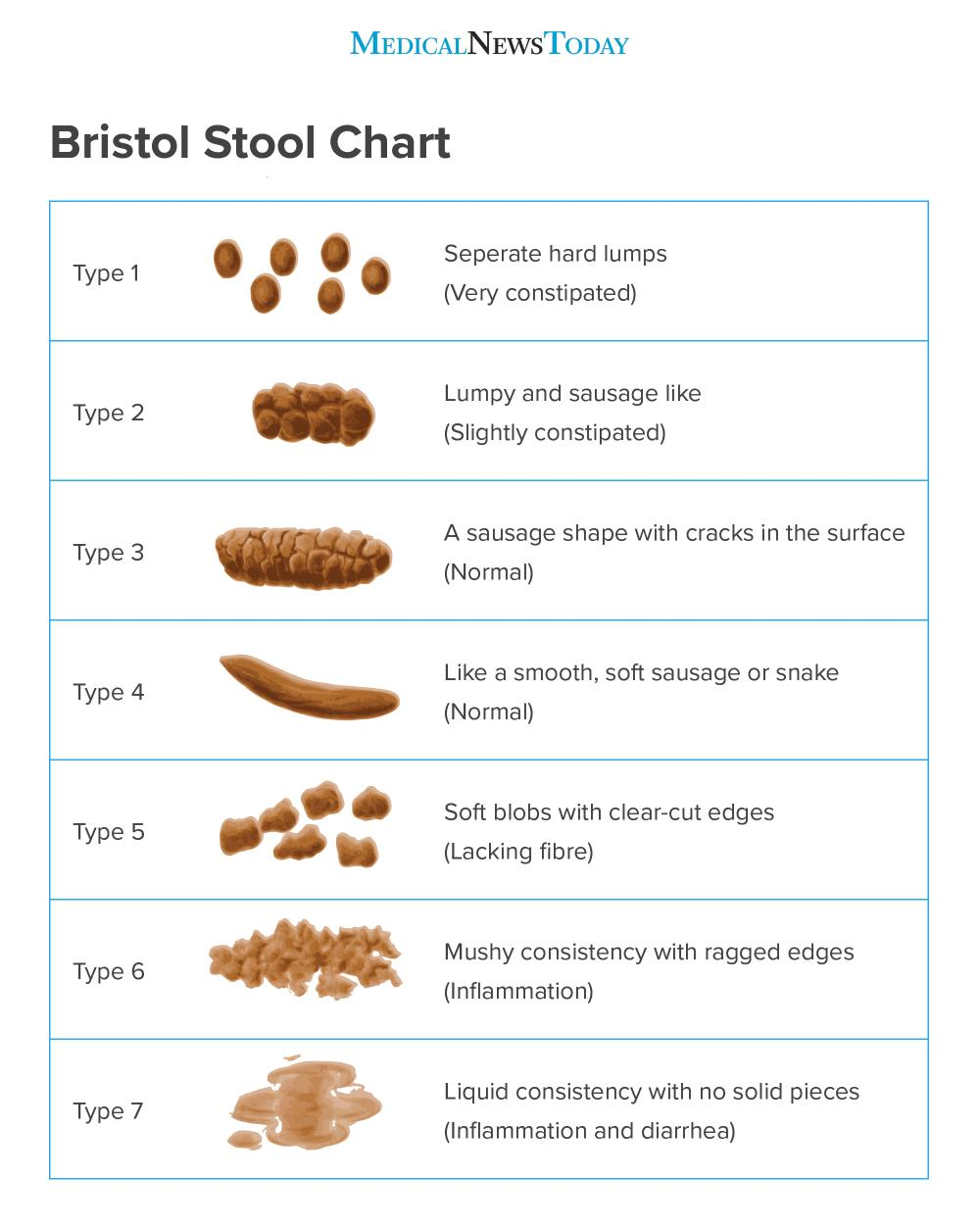
- What does your stool look like if you have IBS?
Stool for IBS-C is very hard, separated lumps if severely constipated. Stool for IBS-D has a mushy consistency ranging from soft blobs to no edges at all. People with IBS-M, or mixed, often see stools ranging from very hard to very soft, as shown in the Bristol Stool Chart below.
- Is it IBS or something else like colon cancer?
Since IBS is a gastrointestinal disorder that shares many symptoms as other more serious GI and metabolic system related illnesses, it is extremely important to rule out other diagnosis with your physician and communicate if your symptoms change. Additionally, IBS is often present in conjunction with other conditions like SIBO or endometriosis, which can and should be treated alongside IBS. Some symptoms not characteristic of IBS are anemia, blood in the stool, unexplained weight loss, fever, and symptom onset after the age of 50 (and not attributed to having your gallbladder removed).
- What are the risk factors for developing IBS?
- Gender (women)
- Changes in the microbiota
- Recent antibiotic use
- Family history (genetic predisposition)
- Food poisoning or a stomach virus
- Lifestyle changes (work, finances, family, relationships, etc.)
- Emotional Stress (recent or past)
- Bacterial gastroenteritis (campylobacter)?
- SIBO
- Dysbiosis
- Pregnancy
- Smoking
- Alcohol consumption
- Food intolerances
- Antidepressants
- Some autoimmune diseases or metabolic conditions
- Can you suddenly develop IBS?
Yes and no. With any functional gastrointestinal disorder, you can consider your stomach and gut as your body’s “weak spot” where you are more likely to be affected when stressed or sick. People with IBS have a predisposition, often genetically, in their gut for sensitivity which becomes triggered during stressful life events, after a bacterial or viral infection, etc. that turns on symptoms. As a result, it is important to avoid triggers by managing stress, eating a healthy fiber-rich diet, exercise regularly at medium intensity, and maintain emotional stability as much as possible.
- Women are twice as likely to have IBS than men in the United States. - Tweet this
There are a lot of connections and research developing about the hormonal tie to digestive disorders and women. Because women’s hormones fluctuate on a much more frequent and regular basis than men, opportunities for bloating, diarrhea, abdominal cramps, nausea, mood swings, and anxiety can be monthly triggers for a flare-up. Some researchers also list the fact that women’s colons are about 8 cm longer than men and extra loopy (making it harder to push things through) is why IBS-C is more common in women compared to IBS-D in men.
- What foods trigger IBS?
Every person with IBS has a different experience, though foods that lead to gas, bloating, or diarrhea can be especially hard to tolerate. The most common culprits are high fat things like dairy products, fried foods, and meat, and insoluble fiber such as raw, cruciferous vegetables like broccoli and cauliflower. Processed foods containing lots of sugar (including artificial sweeteners), chocolate and coffee containing caffeine, and whole grains or gluten have also been found to give people with IBS trouble. Writing a food diary for at least 3 weeks where you record what you eat and how it affects you will help identify foods that may trigger symptoms. It can also be helpful to return to a food diary when having a flare-up because triggers may change over time.
Helpful foods that provide gentle fiber and protein for people with IBS include:
- fruits like kiwi, honeydew melon, cantaloupe, and strawberries
- vegetables like lettuce, carrots, cucumbers, bok choy, turnips, potatoes, and eggplant
- proteins like tofu, tempeh, modest amount of beans, and dark leafy greens
- plant-based milks
- Can celiac disease, lactose intolerance, and other food allergies and sensitivities make IBS worse?
Yes, lactose intolerance and celiac disease or even gluten sensitivity are very common in Western diets and can amplify the symptoms of IBS because they are difficult to digest for an already sensitive system.
- Is IBS worse at night?
Not necessarily. IBS symptoms don’t operate by time of day, rather most commonly by meal size. To avoid abdominal cramping, diarrhea, vomiting, and sleeplessness, try to eat small meals throughout the day. If you can’t, try making lunch your most sizable meal so your body has time to digest before bed-time.
Women and IBS
- Fluctuating hormones during menstruation have been linked to IBS symptoms.
Due to more regular hormonal changes, women report more painful menstruation (dysmenorrhea) and premenstrual syndrome (PMS) compared to those without IBS. Doctors don’t know exactly why yet, but they do know that the spike in ovarian hormones triggers general gastrointestinal changes often leading to increased diarrhea, bloating, and fatigue. Resting, light exercise, and eating hormone-balancing foods such as dark chocolate without traces of lactose, walnuts, and bananas.
- Up to 42% of patients with PCOS also have IBS, according to a 2009 study.
The medical community has found links with both conditions that stem from the microbiome. As a result it is unsurprising that they often occur together and have similar symptoms. Studies also show that when IBS is present with PCOS, a woman’s BMI and percent body fat is likely to be higher and can create a cycle of symptoms. Doctors don’t know yet whether one causes the other, which is why if you continue to have symptoms after cutting out dairy and have been checked for a gluten sensitivity, you likely have an underlying condition which must be treated, such as PCOS.
The Perfect Stool Podcast has two great episodes about the microbiome, women’s health and hormones if you’d like more information: Polycystic Ovary Syndrome (PCOS) and the Microbiome and Gut Testing, Gut Balancing, Hormones, Fertility and Genetics.
- Pregnancy complications
Although every pregnancy is different, the elevated levels of ovarian hormones and the physical pressure the baby puts on the intestines as it grows mean your motility and symptoms will likely change - sometimes for the better, other times not. If diarrhea goes on too long it can cause dehydration, which may lead to serious problems like preterm labor. Constipation can affect the muscles, tissues, and nerves in your pelvis and in extreme cases can cause the uterus to slip out of place.
- Pregnant women with IBS are also at a higher risk of miscarriage.
Additionally, research in some studies show a small increased risk00217-0/pdf) of miscarriage (7%) or ectopic pregnancy (0.74%). It is very important to have a healthcare provider well versed with IBS to help manage and reduce risk, reduce stress as much as possible, and speak with your doctor about any medications for IBS you may be taking.
Complications of IBS
- Impacted bowel
Fecal impaction is a severe bowel condition in which a hard, dry mass of stool becomes stuck in the colon or rectum, blocking passage and causing a buildup of waste. It requires medical attention as soon as possible as it can become life-threatening. An impacted bowel can happen from:
- Overuse of laxatives because your body becomes dependent and can’t pass stool on its own.
- Diet low in fiber (less than 30 grams a day can cause constipation)
- Not drinking enough water.
- A sedentary lifestyle.
- Ignoring the urge to defecate.
- Anal fissures.
- Hemorrhoida.
- Certain medications (opiate analgesics, anticholinergic agents, calcium channel blockers, antacids, and iron preparations).
- Hemorrhoids
Hemorrhoids are swollen veins located in the anus or the lower part of the rectum which can cause bleeding during a bowel movement. Reports show 18% to 33% of people with IBS have hemorrhoids due to straining during a bowel movement, a low-fiber diet, and sitting for long periods of time.
- Malnutrition
Malnutrition due to avoidance of triggering food commonly found on the Low FODMAP diet can become a problem for some people with IBS because these foods contain essential nutrients that are important for health maintenance. For instance, avoiding foods rich in fermentable oligo-, di-, monosaccharides and polyols (FODMAPs), which include wheat, rye, vegetables, fruits, and legumes, may lead to poor nutrition. Many of these FODMAPS, or carbohydrates, are beneficial, acting as prebiotics that stimulate the proliferation of healthy gut microbes. To make sure you are getting the proper amount of nutrients and managing your IBS, it is important to continue to eat 30 grams of cooked fiber a day (both soluble and insoluble), smaller meals, and drink lots of water.
Find out your Personalized IBS Nutrition Plan based on your entire health picture from age, gender, and other existing conditions by taking the quiz here.
- Small Intestine Bacterial Overgrowth (SIBO)
Because IBS has been confirmed to be a disease of the microbiome, it is very common to show up alongside small intestine bacterial overgrowth (SIBO). Many of the symptoms for SIBO and IBS are the same, so it is important to get tested and work with a healthcare provider to manage through a microbiome-recovery based treatment plan.
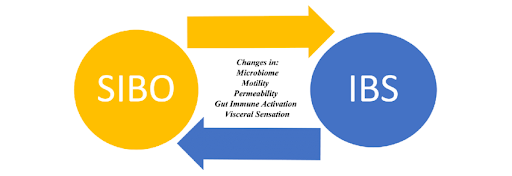
Scientific Figure Chart from The Gut Microbiome and Irritable Bowel Syndrome.
- Impacted quality of life
IBS can come on suddenly. They can be triggered by many environmental, emotional, and psychological factors and as a result people with IBS report needing to restrict their usual activities due to their health an average of 20% of the calendar year. For people with severe IBS, the number increases to 38% of the year.
- Missed work or school
When not managed IBS can have a cascading effect on work, school, or other important responsibilities and cause a cycle of stress. Studies show that more than 25% of people with IBS tend to arrive late or leave early from work or school due to an episode, which is more than one day every other week. Unsurprisingly and unfortunately, the severity of IBS symptoms also has a direct impact on employment. In a survey of people with IBS, between 13%-30% were jobless or unable to work due to the severity of their symptoms.
It is very important to be in a supportive work environment.
- Increased anxiety or mood disorders
With IBS it can seem that you’re happy one minute and grouchy the next, or unable to stop cyclical anxious thoughts. If you’ve ever wondered whether you were imagining it, or tried to get yourself under control without success, rest assured that the explanation is in your gut, and it can be improved. How? Serotonin. Recent studies have shown that about 90%-95% of serotonin is produced in the gut. Serotonin is an important neurochemical that the brain needs to complete physiological and mental processes, such as GI movement and mood. When the microbiome isn’t producing properly, mood disorders like anxiety and depression often show up. The Gut Loving Podcast has a great episode on Anxiety and IBS expert Chloe Brotheridge, and you can often find comfort in cognitive behavioral therapy (CBT) or gut-directed hypnotherapy in the

- Dehydration
Most commonly a concern for IBS-D types, drinking water is very important to all three types to help move stool through the GI tract when constipated as well as replace what has been lost from an episode of diarrhea.
- Pelvic prolapse
Pelvic organ prolapse is when the muscles and tissues supporting the pelvic organs (the uterus, bladder, or rectum) become weak or loose. This allows one or more of the pelvic organs to drop or press into or out of the vagina or anus. Some studies show women with IBS are more likely to report symptomatic pelvic organ prolapse (as well as sexual dysfunction), and report lower quality of life. Prolapse is usually easy to become aware of on your own (from the protrusion, difficulty with leaking urine or feces, or pressure) and is treatable by a medical professional.
- Anal fissures
Anal fissures are small tears in the lining of the opening of the anus. They can be painful, particularly during a bowel movement and is diagnosed by bleeding, either on the stool, on your toilet paper, or in the toilet. Anal fissures are preventable with adequate hydration and a fiber-rich diet. They are also treatable and with any bleeding in the stool it is important to see your healthcare provider right away as it can be a sign of a serious underlying condition.
- Thyroid complications
Although no direct correlations have been found that problems with the thyroid cause or are a result of IBS, they can be similar to SIBO in that they often show up alongside IBS. Why? The microbiome is an endocrine organ, meaning it produces hormones for the body to use and function properly. It is increasingly common to find the microbiome is tied to hormone-related issues like metabolic disease, thyroid issues, and more. Hypothyroidism, when the thyroid gland doesn’t produce enough hormones and often found with IBS-C and SIBO, share many of the same gastrointestinal symptoms: constipation, bloating, and cramping. Hyperthyroidism, when the thyroid produces an excess of hormones and is often associated with IBS-D, shares many of the same symptoms: increased bowel movements, anxiety, and more.
- Metabolic syndrome
Metabolic syndrome is a cluster of conditions that occur together, increasing your risk of heart disease, stroke and type 2 diabetes. These conditions include increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels. Recent studies have shown a positive link from IBS to metabolic syndrome especially in middle-aged people.
Actionable steps to prevent and manage IBS
Regularity is key. Practicing healthy habits is key to avoid a flareup or get you through one with as minimal symptoms as possible.
To begin healing the gut from IBS, it is important to build up microbiome diversity. Start by removing triggers such as dairy and gluten for one month, and getting tested for celiac’s disease and gluten sensitivity. A leading gastroenterologist treating IBS in Long Beach reports 50% of patients experience total resolution of symptoms at this point.
If symptoms are not resolved after eliminating dairy and gluten, there is likely an underlying cause and it is important to find and treat (hormonal, bacterial infection, fungal, etc.).
Although a microbiome-building protocol is based on common low-risk best practices, it’s best to speak with your doctor first, especially before starting a big change like a low FODMAP diet. At WeTheTrillions, we work with the best-trained clinicians to ensure you get meals tailored specifically to help with your symptoms and tackle their root causes. You can review what some of those options look like here.
- Eat a healthy microbiome diet.
We know that a signature of IBS is the change in microbiome bacteria so keeping it as healthy and diverse as possible is essential with good gut bacteria feeding food. Avoiding gut-compromising foods that do not increase microbiome diversity, such as animal products, alcohol, refined sugar, refined oil, and environmental toxins are a great place to start to prevent IBS. If you already have IBS, make sure to also avoid caffeine, carbonated drinks, and gluten for some to begin managing it. To build up the microbiome and start healing, focus on cooked starchy fruits and vegetables, and simple carbohydrates in phases.
- Phase 1: starchy, frozen vegetables (carrots, turnips, potatoes), soluble fiber fruits.
- Phase 2: whole grains (quinoa, oats).
- Phase 3: fermented foods (sauerkraut, kimchi).
- Phase 4: raw vegetables (lettuces, beans).
- Cooked food is 16x more efficient for our digestive systems to use than raw food.
For people with IBS, this can make a big difference in healing and managing when you have a flareup. - Tweet this
- One of the biggest things to keep in mind with dietary changes: It’s best to plan ahead.
It can be difficult to start a new diet and stick with it if you don’t understand how you’ll integrate the changes into your life. Below are a few things to think about when getting ready to implement some dietary changes:
- Get rid of foods that trigger your IBS symptoms. This list will likely come from your food diary that you discuss with your doctor.
- Create a list of go-to foods that will ensure you get the nutrients you need.
- Consider opting for an IBS-focused meal delivery program that can take the guesswork out of what foods will help alleviate your symptoms.
- Reduce diarrhea by avoiding triggers.
Dietary changes are another way that those with IBS can reduce diarrhea. The following diet-specific tips are recommended to reduce diarrhea:
- Avoid chocolate, fried foods, alcohol, caffeine, carbonated beverages, products with sorbitol (found in sugarless chewing gum), and fructose.
- Eat soluble fiber, which is often found in chia seeds, oat bran, barley, fruit flesh, along with navy, pinto, and lima beans.
- Drink water an hour before or after meals rather than while you eat. Drinking during meals causes the food to move through your digestive system quicker.
- Reducing constipation by avoiding food triggers.
Another IBS symptom that can be helped with a slight shift in diet is constipation. If you are suffering from constipation, the following tips are recommended:
- Meet minimum daily fiber requirements (25 grams for women, 38 grams for men).
- Slowly increase your intake of high-fiber foods like whole-grain bread, cereals, fruits, vegetables, and beans.
- Try incorporating dried plums, prune juice, and ground flaxseed into your diet.
- Avoid alcohol, coffee, carbonated drinks, and processed foods such as cookies, chips, and white bread and rice.
- Drink 8 glasses of water a day.
Water is beneficial for IBS for several reasons. First, for people who are diarrhea dominant, they need to replace the water exiting their body too fast and are at a higher risk of dehydration. For people who are constipation dominant, water helps move dried out stool through the colon for more regular bowel movements and less bloating.
- Watch portion sizes.
No, it has nothing to do with weight loss. The neurotransmitters in the lining of the gut are hypersensitive in people with IBS so eating too much food too fast can be aggravating. Your gastrocolic reflex, a physiologic response that makes room for the food you’re eating, gains strength in direct correlation to the number of calories you consume in a meal. - Tweet this.
Some people with IBS find that eating smaller meals throughout the day helps limit cramping and other common stomach problems, which is why here at WeTheTrillions offers both full meals and snacking options.
- Holding it in instead of having a bowel movement.
Trying to wait to have a bowel movement can cause excessive fermentation and a build-up of gas in the colon. Cue additional bloating and cramping. It’s best not to fight it and use the restroom whenever you have to.
- Low or medium intensity exercise: swim, dance, walk, cycle.
The importance of exercise to improve IBS symptoms lies in stimulating the parasympathetic nervous system (also known as the “rest and digest” system) to begin relieving the chronic stress that people with IBS have. Increased exercise helps blood flow to the digestive system, especially low-intensity aerobic exercise like yin yoga, walking, swimming, or riding a bike for a minimum of 3x a week (30 minutes each) up to 5x a day (up to 60 minutes).
- Practice yin yoga regularly.
Studies have shown that because yoga focuses on the mind-body connection, and poses can be easily modified, it’s perfect to soothe IBS symptoms like constipation and bloating to keep the condition in remission long-term. Yin yoga where you dwell in each pose for several minutes is specifically good because it is low-medium intensity. It strengthens the body in a low-stress way helping to avoid the stress hormones that are triggered during high intensity exercise that can make IBS symptoms worse.
Yoga With Adriene on YouTube has two playlists that focus on Gut Health and Digestive Flow. Within each are several videos ranging in focus for the body, length, and intensity.
- Build good sleep habits.
Regular exercise also helps you sleep, and sleep is important because that’s when your body sleep is able to make and use serotonin.
Here are some tips for getting a better night’s sleep:
- Set up a proper routine before bed. This can include dimming the lights and turning off technology.
- Go to bed at the same time every night.
- Try to avoid napping during the day.
- Wake up without an alarm clock and get up immediately after waking. This can help you get into a natural routine. If you feel you need an alarm clock, you may find a sunrise alarm clock useful. These clocks are designed to mimic the sunrise to wake you up in a more natural way.
- Don’t drink caffeine after 2.00 pm and avoid alcohol close to bedtime.
- A relaxing bath and a hot drink can also help you relax.
- Avoid light from your computer and phone at least 30 minutes before going to bed.
- Melatonin supplements have also shown initial promise in some studies not only in helping improve sleep but in reducing IBS-D symptoms.
- Supplements and medication may be necessary.
Most people don’t have a chronic form of IBS, but depending on the severity of your symptoms, your doctor may speak with you about supplements and medications that can help reduce symptoms.
- For constipation, increased probiotic strains: B. infantis 35624, L. rhamnosusGG, S. boulardii.
- For diarrhea, increased probiotic strains: Lactobacillus strains (such as L. acidophilus, L. plantarum, and L. casei) and Bifidobacterium strains (such as B. infantis, B. longum, and B. bifidum).
- Antispasmodics for cramping.
- High dose vitamin C or laxatives, when necessary.
- Ayurvedic medicine to regulate motility (such as Triphala)
- Digestive enzymes or digestive tea.64. Check with your doctor about medications that may be causing IBS.
Some people's IBS can be traced to food poisoning or food sensitivities, while others may be hormonally related. If you have adopted a healthier lifestyle and are still experiencing symptoms, it’s possible one of your medications is causing IBS symptoms and you will need to work with your doctor on changing your treatment options if possible.
- Prioritize mental health and stress management.
We can all find ways to reduce stress in our everyday lives. Whether it’s learning not to take on more work than you can handle, cutting down on socializing, or getting into an organized routine, there’s something you can do to make your lifestyle less stressful overall.
Some further suggestions you may find helpful are:
- Exercise regularly.
- Learn to manage time more effectively.
- Make time for hobbies and interests.
- Seek out social support when needed.
If these minor steps don’t work, there are more extensive programs that you could introduce. Cognitive-behavioral therapy (CBT) can be highly beneficial to people with IBS. According to research, a tailored CBT program can be more helpful than some medications or even the low FODMAP diet for people living with IBS.
- Meditation can help improve IBS symptoms.
Meditation takes different forms and has shown to be helpful for women with IBS. Whether you prefer breathing techniques or guided meditation, there’s something out there for you. You can choose from audio CDs, meditation cards, or a meditation app.
- Progressive Muscular Techniques to aid in relaxation.
This involves tensing and relaxing each of the major muscle groups. Sometimes this will start with your feet and work up to the head and facial muscles, or start with your upper body and work downward.
You hold each muscle for a few seconds and then let it go. This technique can reduce overall body tension and is good to practice before bed. You can find instructions for it here.
- Visualization techniques can help reduce stress.
If you’re feeling stressed and tense, visualizing yourself in a relaxing setting like a beach, a tropical forest, or the countryside can help you unwind. You can find directions on how to do this by following the above link or simply create your own visualizations.
- Acupuncture is a promising treatment combined with lifestyle changes for IBS-D.
Several studies have shown an improvement in patients with diarrhea based IBS from acupuncture over a several week regimen. Combined with lifestyle changes and stress management, the medical community currently views the combination of Chinese herbal medicine with conventional Western medicine as a promising treatment for IBS-D that deserves continued research.
- Gut-directed, clinical hypnotherapy
In a study in the Journal of Clinical and Diagnostic Research from 2016, researchers found “psychological intervention, particularly hypnotherapy, alongside standard medical therapy could contribute to improving quality of life, pain and fatigue, and psychological disorder in IBS patients resistant to treatment. Also, therapeutic costs, hospital stay and days lost from work could be decreased and patients’ efficiency could be increased.” Another study found gut-directed hypnotherapy to have a similar efficacy as the low FODMAP diet.
Jump to
Patient Advocacy and Support Groups
- The IBS: It’s a Pain Reddit Channel is perfect for scrolling when the bathroom is “occupied.”
It is just the right blend of funny and thoughtful, first-person advice.
- Facebook Groups offer every style of support you need.
There are lots of Groups to choose from, whether you’re looking for purely clinical, evidence-based, specific to women, around the world, or alternative medicine. You’ll find it below.
- IBS Patient Support Group created by IBSPatient.org
- At over 61,000 members, the IBS Support (Official) Facebook Group is one of the largest and most active support groups for people with IBS, strictly adhering evidence-based, clinically researched advice and sharing.
- Since IBS affects slightly more women than men and as a result have some unique hormonal elements to consider with IBS, you may consider joining the 13,000-strong IBS Support Group For Women on Facebook. - Parents of IBS Kids - Pediatric IBS Support Group is helpful for learning tactics to support a child with IBS.
- IBS-C / SIBO-C / Constipation / CIC/ Methane Dominant Support Group. As the group states, “the motivation behind creating a separate group for C is the fact that the treatment options, research and symptoms for this type of SIBO/IBS are so different than SIBO-D.”
- IFFGD, the International Foundation for Functional Gastrointestinal Disorders, is a charity working to educate, advocate, and support patients, families, physicians, nurses, practitioners, investigators, regulators, employers, and more about disorders like IBS.
Read their newsletter for the latest in medical research, clinical trials, and patient advocacy on Capitol Hill.
- IBS Patient Group is a nonprofit community that created #WorldIBSDay on April 19th to educate and inform people about the prevalence of, treatments for, and clinical trial opportunities available.
Join the support group here.
- Many hospitals and healthcare providers in your community may also be able to direct you or someone you know to local groups.
You can also try searching for a Meetup Groups about IBS in your area.
Useful Apps
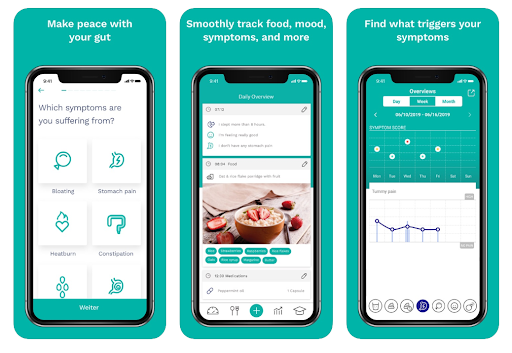
- Bowelle - The IBS tracker
Bowelle is a food and symptom diary to help people with IBS discover patterns and changes in symptom management from mood to bowel movements to stress and more over time. The benefit of this app is it can easily export your data via email and share it with your doctor, nutritionist or dietitian. Bowelle also syncs with the Apple Health app and is free on Apple.
- Cara: Food, Mood, Poop Tracker for IBS, IBD, and GI Health
Monitor your digestive health to learn more about the connection between your mind, gut, nutrition, and overall well-being. Free for iOS and Android, Cara lets you track food (including sensitivities and allergies), stress, poop, tummy pain,exercise and individual factors to discover your body’s triggers and create a personalized health diary. It also syncs with the Apple Health app.
- mySymptoms Food Diary App - for discovering personalized food sensitivity trends
mySymptoms helps you discover what food triggers you by recording, tracking, analyzing, and reporting on your diet and symptoms. The best part is with a few simple taps, you can track your favorite foods (along with sleep, medications, etc.), input the severity of symptoms experienced, and then run the analysis to identify patterns that emerge. As you track your diet and symptoms, the app provides summary and trends charts that plot both frequency and intensity, making it easier for you to discuss with your doctor. Find it on Apple or Android for $2.99.
- Food Intolerances App - Histamine, FODMAPs & IBS Guide
Listed as a Healthline Best Nutrition App 2019, the Food Intolerances app helps people who have to stick to a restricted diet like IBS, SIBO, leaky gut or endometriosis because of food intolerances or allergies. Typical application cases are: histamine intolerance, mastocytosis, fructose malabsorption, sorbitol intolerance, aspirin intolerance, gluten sensitivity, lactose intolerance or a diet low in FODMAPs. Find it on Apple for $6.99 or Android for $4.99 and get a deep insight into your food intolerances and suggestions to avoid for better gut health.
- Monash University Low FODMAP Diet App
Leading much of the research on GI health and IBS, and developers of the low FODMAP diet, researchers at Monash University have developed an app to assist in management of the gastrointestinal symptoms associated with Irritable Bowel Syndrome (IBS). Offering tutorials to guide you through the 3-Step FODMAP diet and reintroduction phase, a “traffic light system” detailing the FODMAP content for hundreds of foods and their measurements, and a shopping list function, the Monash App is $9 on Android and $7.99 on Apple.
- Moodfit: tools and insights to shape up your mood
Available on Android and Apple, Moodfit is a free mental health app whose tools and insight are meant to “shape up” your mood. Whether you’re looking to better understand your feelings, or you’re experiencing anxiety, depression, or high levels of stress, Moodfit allows you to track your moods and over time determine what types of things affect your feelings—like sleep, medication, and exercise. The cognitive behavioral therapy skill building and the ability to run your own experiments - for example if you suggest gluten or dairy may be having a poor effect on your body - really make this app one of a kind in identifying what treatment strategies are working best for you and your unique picture.
- TalkSpace for flexible talk therapy
TalkSpace has 1 million users and is an app (for your phone, tablet, or computer) that first matches you with a relevant, licensed therapist to whom you can send unlimited text, voice, video, or photo messages any time of day or night. Your therapist isn’t “on call” to respond immediately (though they do respond 1-2 times a day), but having the ability to bring up an issue whenever it suits you can be helpful to relieve the stress in the moment. Depending on the plan you choose, you can schedule live conversations up to several times a month, starting at $65/week.
- BetterHelp for flexible talk therapy
With more than 1,500 licensed therapists on board, BetterHelp is the world's largest e-counseling platform available on Apple, Android, and desktop. Choose to message, chat live, hop on the phone, or video chat with your therapist an unlimited number of times per week, though similar to TalkSpace they are not “on call” without a scheduled appointment. Prices range from $40 to $70/week.
- Happify: for Stress and Worry
Happify’s science-based activities and games can help reduce stress, overcome negative thoughts, and build greater resilience by providing effective tools and programs to improve emotional well-being. Techniques are developed by leading scientists and experts who've been studying evidence-based interventions in the fields of positive psychology, mindfulness and cognitive behavioral therapy for decades. Happify also lets you decide which track you’d like to work on from coping better with stress to achieving mindfulness through meditation, conquering negative thoughts, and more. Download it for free on iOS and Android, or upgrade to full features for $11.67 a month.
- Cognitive Behavioral Therapy and Mediation - Sanvello: On-Demand help for stress, anxiety, and depression
The Sanvelllo app is based on the principles of cognitive behavioral therapy (CBT) and mindfulness meditation, strategies shown to provide clinically validated relief for mental health concerns including anxiety and depression. Additionally, in a randomized study of 500 adults with mild to moderate anxiety and depression, the tools offered by Sanvello were shown to decrease symptoms. The effects lasted even after participants stopped using the app. A basic version is available on Apple and Android, and there is an upgrade version for $8.99 covered by some insurance plans.
- Meditation - Aura: Personalized Mindfulness
The Aura app is a simple, personalized solution to reduce stress and increase positivity through 3-minute meditations, customized to you by Artificial Intelligence. Do you wish to control your stress and thoughts better? Have you tried other mindfulness meditation apps but couldn't form a habit around them? Learn how to reduce stress, control your emotions better, and build habits that stick with several free meditations, daily gratitude reminders and more. Premium unlocks additional meditations, integration features, and offline downloads for $11.99/month. Available on both Apple and Android.
- Stop, Breathe and Think - Personalized Meditation
Stop, Breath and Think (SBT) ia another app offering a personalised meditation and mindfulness experience complete with guided sessions, journaling and more. Winner of the 2017 Webby People’s Voice Award for Best Health App, a recent study saw a 22% decrease in users feeling anxious after just 10 short sessions. Available to download for free on Android and iOS with several activities, or upgrade to unlimited activities for $9.99/month.
- Headspace for meditation
Headspace, used by millions around the world, is all about mindful meditation. There are a variety of sessions on everything from stress and sleep to focus and anxiety. There are even exercises for how to get through an emotional crisis exactly when you need it. A 10-day free trial helps users practice the basics of meditation and a monthly subscription of $12.99 on Apple or Android helps build and maintain healthy emotional habits whether you have 5 minutes or an hour.
- Yoga for mind and body
The key here is less about which poses you do, and more about how often you practice. Low intensity yin yoga at least twice a week has been shown to improve IBS symptoms over a twelve-week period, on it’s own and combined with other lifestyle changes like a healthy diet. Whether you’re at home, traveling, or at work, these apps can help make yoga a regular part of your healing practice.
- Yoga Studio: Mind & Body - This combined yoga and meditation app features over 130 videos and meditations ranging from 5-60 minutes. Find the right class for your health needs or build your own class pose by pose. Quickly search and download classes based on intensity, ability, and duration, or browse the featured collections. Available on iOS and Android, subscriptions range from $5-10 a month.
- Daily Yoga: Workout & Fitness - With hundreds of curated classes for various fitness goals, step-by-step instructions for every pose, and a global community to stay motivated, this regularly updated app is available on iOS and Android. The free version offers minimal, so if you choose this app, a subscription ranges from $3.33-19.99 a month for the Pro Plan.
- Find What Feels Good (by Yoga with Adriene) - Offering 100+ hours of yoga videos and mediations ranging in length and focus (gut health, digestion, adrenal fatigue, menopause, calm core, and chakras are just a few yoga sessions), the FWFG app can automatically beam from your phone to your Chromecast or AirPlay enabled devices, or download to watch offline. for later use. A subscription is $9.99 a month on iOS and Android.
- FIT ON: Free Fitness Workouts
With unlimited access to workout classes ranging from low intensity cardio to mid-intensity strength training, yoga, Pilates, dance, barre and more - FIT ON is a free app of fitness videos from top celebrity trainers like Cassey Ho (of Blogilates), Jeanette Jenkins, Katie Dunlop (of Love Sweat Fitness), Christine Bullock, Kenta Seki, Danielle Pascente, Caroline Pearce and many more. Set reminders, download for offline use, and track against your health goals. Free for iOS and Android.
- Daily Water Tracker Reminder
Free for iOS and Android, the DWTR enables you to set your daily water intake goal, log it with several fluid ounce options, view a detailed stats update after every glass to see how close you’re getting to your daily goal, or review 7- and 30-day charts for an idea of your overall progress. The alert notifications are fully customizable.
- Aqualert: Water Tracker Daily
Aqualert notifies you throughout the day to keep you properly hydrated, taking into account your activity level to calculate your daily water requirements. Get alerts for unbroken streaks to improve your body’s function, skin, healthy weight and more. Download it for free on iOS or Android.
- Period tracker
Since menstruation can be a trigger for an IBS flare-up and sometimes be associated with other conditions like PCOS and endometriosis, it can be helpful for you and your doctor to track your cycle. Below are some great apps - try them out and see which you like!
- Clue (free for Apple and Android) - clean with exceptional science behind it and a multitude of options for what you can track.
- My Flo ($1.99 for Apple and Android) - Perfect for women with irregular menstruation, women starting menopause, or women wondering why they’re experiencing other symptoms (such as excessive bloating, migraines, constipation, or low energy), My Flo can help identify hormone imbalances and suggests lifestyle changes like the best foods to eat or self care and fitness activities that could make you feel better during your cycle.
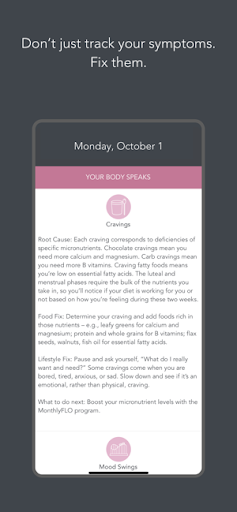
- Period Tracker Period Calendar (free for Apple and Android) - Simple, straightforward in how you track and rate symptoms, and anyone—regular or irregular, newly menstruating or premenopausal—can use it.
- Flo (free for Apple and Android) - record ovulation and period symptoms, and know exactly what your body is doing and when. Flo also turns into a pregnancy tracker if and when you ever need it to.
- Eve, by Glow (free for Apple and Android) - focusing primarily on period tracking, sex life and gym habits, Eve’s clean and colorful icons make tracking your menstrual cycle almost like a game.
- Glow: Fertility Calculator and Ovulation Tracker (free for Apple and Android) - backed by experts like Sheeva Talebian, MD, a board-certified reproductive endocrinologist, Glow allows you to track 40 different health signals including but not limited to sexual activity and body basal temperature, both for those trying to get pregnant or not. It can also help those who are undergoing fertility treatments through their online communities and various resources.
- Gut directed hypnotherapy - Nerva for IBS: Rewire your gut-brain connection
Designed by a clinical gut-directed hypnotherapist, Nerva helps people with IBS rewire the gut-brain connection to reduce and manage their symptoms from home. Based on clinically proven hypnotherapy approach, which was shown in a Monash University study to improve IBS symptoms by up to 80% in 3 out of 4 people, 15 minutes a day for 6 weeks could help improve diarrhea and constipation, and reduce pain. Try practicing hypnotherapy sessions when it's convenient for you, no appointments, no waiting lists for a measurable improvement. The Nerva program is available for $159 one time only for the entire 6-week program. Could be worth trying it out!
Read the clinical trial on the efficacy of clinical gut-directed hypnotherapy versus the Low FODMAP diet.
- Happy Inside – IBS Hypnotherapy
Founded by Michelle White, psychotherapist and clinical hypnotherapist in Sydney, Australia where many of the cutting edge therapies for IBS are being developed, the Happy Inside program is now a fully online program of resources and support for people experiencing gut disorder and chronic conditions. The app - for iPhones at $5.99 - was built on 9 years of clinical experience in gut focused therapy to address unresolved stress, anxiety, emotions and life misalignments to regulate the central nervous system (vagus nerve, also known as the gut-brain axis) to decrease pain and digestive disorders, enabling you to improve your relationship with your body, gut, food and self.
- Public bathroom locator app: Flush - Toilet Finder & Map
Flush has over 190,000 bathrooms around the world in its database, including details like whether or not it’s handicap accessible and if you need a key to use it. It even allows you to search for a bathroom without an internet connection- perfect for traveling! The Flush app is free and available for iPhone and iPad (requires iOS 8.0 or later) as well as Android devices, and provides an instant map of all available bathrooms in your area.
- Worldwide bathroom locator app: Bathroom Scout
Bathroom Scout provides the locations of over 2 million restrooms worldwide, including public bathrooms and those in restaurants and other facilities (service may be required before use). It is available for $0.99 on Apple (requires iOS 4.3 or later) and Android devices. Turn-by-turn navigation and street view lead you exactly where you need to go.
- Bathroom Noise Distractor: HushPoopy or Fake a Shower
If you have “Poo Pride”, good for you! If you don’t, Hushpoopy for iOS is a free app that helps cover the sound of your bathroom visit with a range of noisey choices: hair dryer, shower, rain and thunder, dryer machine, and more. Fake a Shower is a similar free Android app version with shower and faucet choices, that can even tell you how many liters of water were saved by not actually turning on the faucet!
IBS in numbers
- Irritable Bowel Syndrome affects 10-15% percent of adults.
That’s 25-45 million people in the United States, yet up to 75% of patients are undiagnosed or may lack a formal medical diagnosis of IBS. - Tweet this
- Twice as many women as men have IBS.
Since we don’t quite know what causes IBS in the first place, research is still investigating why women tend to have it more often than men. However, since gastrointestinal disorders disproportionately affect women, recent studies offer the following as potential reasons: seeking a diagnosis rather than "toughing it out", hormonal changes, and sex-related differences in brain structure (the nerve cells that control the movement of food through the intestines are potentially more sluggish in response to brain inputs in women than in men).
- 35-40% of patients have moderate IBS.
According to AboutIBS.org, 25% have severe IBS.
- Between 4-78% of IBS patients have SIBO.
Variation in the methods to diagnose SIBO is the most important reason for the wide variation in frequency of diagnosis among patients with IBS. Listen to the Low FODMAP Diet and IBS Podcast to learn more about the differences and and how they're diagnosed.
- 50-90% of those who seek treatment for IBS also struggle with an anxiety disorder of depression. - Tweet this
According to the Anxiety and Depression Association of America, it is one of the most common complaints about IBS symptoms.
- IBS accounts for up to 12% of total visits to primary care providers annually in the United States.
That makes the most common disorder diagnosed by gastroenterologists.
- The cost to society of IBS for direct medical and indirect lost productivity is estimated at $21 billion or more annually.
According to the IBS Global Impact Report 2018, there was a loss in productivity by people diagnosed with IBS by 31-33% loss compared to 19.6% for people not diagnosed with IBS. Additionally, IBS interfered with their productivity and performance during an average of nine days per month, causing some to miss school or work for an average of two days per month.
- Prior to a diagnosis, 3 out of 4 patients in the US report having tried an average of 3.6 over-the-counter products before speaking to a healthcare provider about their symptoms.
Additionally, the majority of patients reported taking OTC medications for roughly a year before consulting a medical practitioner.
- When asked how IBS-D affects them, 81% stated that they avoided situations where there was no nearby bathroom.
- The American Gastroenterological Association found in a 2016 study that nearly two-thirds (64%) of IBS-C patients and 55% of respondents with IBS-D reported they “avoided having sex” because of their symptoms.
“For women with IBS, an association with painful sexual intercourse (dyspareunia) has been reported since the 1980s, when a study comparing sexual function in women with IBS, inflammatory bowel disease, and duodenal ulcers showed a prevalence of painful sexual intercourse (dyspareunia) in 83%, 30%, and 16% of women respectively.” - IBS Global Impact Report 2018.
Latest research
- Fecal Microbiota Transplantation for repopulation of the microbiome.
Since IBS stems from the gut, the medical community has turned to fecal microbiota transplants (FMT) to investigate if there is a "cure for IBS" to be found by repairing the micriobiome. Several studies have shown early signs of improving symptoms for patients with IBS while others show no change. During an FMT, stool from a healthy donor is processed and then transplanted into a patient's colon to repopulate the gut with a healthier range of microorganisms. Moderate symptoms improvement was reported in 76.9% of those in the lower-dose fecal transplant group and 89.1% of those in the higher-dose group. Additionally, symptoms went away entirely in 35.2% of those in the lower dose group and 47.3% of those in the higher dose group - with 90-95% of patients reporting ongoing improved symptoms one year later.
More research needs to be done to bolster initial results and learn more about the long-term effects on the micriobiome of IBS patients.
- Urine test diagnosing IBS needs further research.
Researchers have recently discovered a difference in the biomarkers in urine from healthy people and those with IBS. Most significantly, there shows a degradation of collagen, likely from the colon wall, which occurs in patients with IBS. More research is needed to see whether the test can be a non-invasive, less costly diagnosis option for doctors and patients.
- FDA approves IBS-Stim device for kids with IBS.
The prescription-only device approved in June 2019 for kids age 11-18 experiencing abdominal pain from IBS is placed behind the patient’s ear. Stimulating nerve bundles in and around the ear has been shown to provide pain relief. The battery-powered device emits low-frequency electrical pulses continuously for 5 days then must be replaced. Patients can use the device for up to 3 consecutive weeks. According to reports, the IB-Stim treatment resulted in at least a 30% decrease in usual pain at the end of 3 weeks in 52% of treated patients.
- Clinical trials on cannabidiol (CBD) are ongoing for IBS patients.
CBD, a non psychoactive derivative of marijuana or hemp, is known around the world for its calming effects in reducing anxiety and chronic pain. Recently the medical community has turned to it to ask whether CBD oil can reduce the pain of abdominal cramps and bolster anecdotal evidence. Clinical trials are currently underway.
Dating and Relationships
Take care of YOU first. In addition to all of the therapies and best practices for managing IBS listed above, here is some advice from the experts about the importance of supportive, healthy relationships and how to maintain good ones.
- Remember, you are not your IBS.
It can be helpful to remind yourself of this from time to time with a personal mantra. Here’s a great article from someone who has used personal mantras to change the way she thinks about healing and strength and instructions for how to write your own personal mantra.
- Successful dating tips for partners with IBS.
Here are several tips for partners, family members, or coworkers of people with IBS and what they can do to help from the International Foundation for Gastrointestinal Disorders:
- Consider the person with IBS as the expert in charge of his or her condition. Do not be over-watchful or over-protective. Asking, "Are you alright? Are you really ready to leave?" can actually provoke a bit of anxiety in someone with IBS, which affects the gut and can lead to a sudden sense of urgency or pain.
- Help create more regularity in home life and time management. Avoiding disorganization, over-scheduling, or lack of planning will help the person with IBS feel more internally regulated and balanced and help restore a sense of control.
- Be flexible. IBS symptoms can flare up at any time without warning. Understand that plans sometimes will need to be changed.
- Avoid (sometimes unintentionally) laying blame on the person with IBS. Saying things such as, "You don't eat right," or "You worry too much," grows out of a desire to help, but places blame. It makes the person with IBS feel less in control because she or he knows how often even the best of self-discipline cannot always prevent an outbreak of symptoms.
- Healing from current or past relationships can help reduce stress and manage IBS.
We don’t yet know all the reasons why the gut-brain axis goes awry and causes IBS, but we do know that both short-term and long-term stress can affect that communication channel and manifest in chronic conditions. Sometimes, understanding, healing, and recovering from a functional medical problem like IBS can be assisted through relational healing with a psychologist.
Work, school, and travel with IBS
Managing your IBS symptoms can be demanding enough in everyday life, but traveling can make management more of a challenge. One of the main reasons for this is because of the way your eating patterns may change while you’re traveling.
To make traveling easier, remember what works for you. You’ll know what contributes to your IBS, so avoid these triggers while you’re on vacation. This may mean having a slightly different routine to any of your travel buddies, but you have to do what works for you.
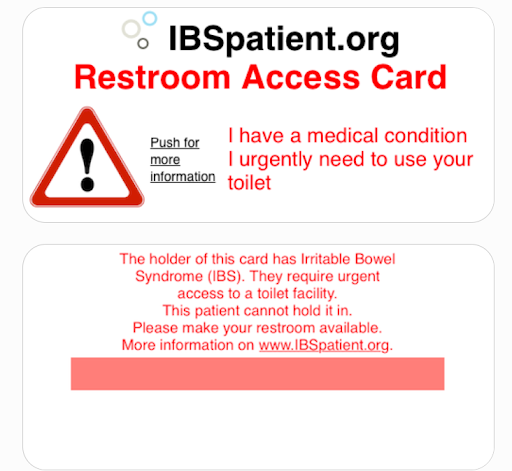
- Be prepared for anything with an IBS Restroom Access Card
Created by IBSpatient.org, showing an IBS Restroom Access Card to a server, flight attendant, or teacher helps communicate your medical condition when you need a restroom quickly. Screenshot the image, or bookmark it here.
- Letter to employer about working from home
Stability in basic needs like employment and access to education are important for keeping stress at bay. As a result, it can be important to let your manager know that while you don't always have control over IBS symptoms, you are a dedicated employee. Symptoms may force you to leave a meeting or go to the bathroom often but affirm that you'll be able to do your job after the pain and discomfort subsides. At times it may make sense for you to communicate your medical needs at work and adjust as needed to a more flexible environment like working from home. To reduce your potential economic loss, IBSPatient.org adopted a letter which you or your doctor can submit to your employer to support working from home.
Books
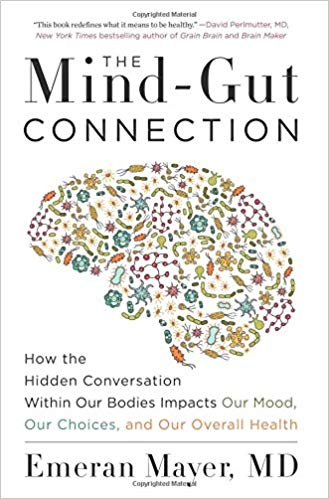
- The Mind-Gut Connection: How the Hidden Conversation Within Our Bodies Impacts Our Mood, Our Choices, and Our Overall Health by Emeran Mayer, MD
Mayer’s research has been supported by the National Institutes of Health for the past 25 years, and he is considered a pioneer and world leader in the area of brain-gut microbiome interactions. Buy it here.
- Gut: the inside story of our body's most under-rated organ by Giulia Enders
An international bestseller from a world renowned scientist! Watch her TEDx Talk in the Documentaries and Videos section below or check out the book here.
- The Second Brain: A Groundbreaking New Understanding Of Nervous Disorders Of The Stomach And Intestine by Michael Gershon
The book is a groundbreaking work and documentary of the same title is available on Amazon Prime in the Documentaries and Videos section below.
- 10% Human: How Your Body’s Microbes Hold the Key to Health and Happiness by Alanna Collen
A biologist, Collen argues that so many of our modern diseases—obesity, autism, mental illness, digestive disorders, allergies, autoimmune afflictions, and even cancer—have their root in our failure to cherish our most fundamental and enduring relationship: that with our individual colony of microbes. The good news is that unlike our human cells, we can change our microbes for the better. Life—and your body—will never seem the same again. Read it here.
- I Contain Multitudes: The Microbes Within Us and a Grander View of Life by Ed Yong
A New York Times Bestseller, Ed Yong takes us on a grand tour through our microbial partners, and introduces us to the scientists on the front lines of discovery. His writing has appeared in The Atlantic, National Geographic, the New Yorker, Wired, the New York Times, Nature, New Scientist, Scientific American, and more.
- The Diet Myth: The Real Science Behind What We Eat by Tim Spector
Spector is a Professor of Genetic Epidemiology at King’s College London and has published over 600 research articles in prestigious journals including Science and Nature. Get his book here.
- More books about soothing constipation, helping children with IBS, and cookbooks are available from the International Foundation for Gastrointestinal Disorders here.
Podcasts
- Butts & Guts Podcast by the Cleveland Clinic
All About Irritable Bowel Syndrome (IBS) with Dr. Christine Lee on the Butts & Guts Podcast is worth all of the 22 minutes, this podcast explores digestive health from end to end. In this episode, gastroenterologist Dr. Christine Lee, explains what irritable bowel syndrome (IBS) is and how common it is compared with other disorders affecting the GI tract, as well as measures that can be taken to control the condition.
- IBS Chat Podcast by IBS Patient Support Group
Episodes of the IBS Chat Podcast include conversations with Patients, GI Researchers and Healthcare Providers on topics which are geared towards an IBS sufferer. The podcast series covers the tests for IBS (including a blood test), mindfulness techniques by psychologists, the latest clinical research on IBS and children, pets, cannabis, etc.
- Episode 9: Mindfulness-based psychologist Jennifer Franklin Ph.D. who created DontHateYourGuts.com to help patients be inspired to seek healing discusses how therapy can help heal people with functional GI disorders.
- Episode 4: Dr. Pimentel is a pioneer in motility disorder research having discovered a blood test to provide a definitive diagnosis for IBS. He is the Program Director of MAST at Cedars-Sinai Medical Center and talks about what the role of SIBO plays, the changing methods of diagnosing based on inclusion versus exclusion, and how food poisoning is a very common trigger for IBS that can now be tested.
- The Perfect Stool: Understanding and Healing the Gut Microbiome by Lindsey Parsons
From interviews with functional and integrative medicine professionals, patients and scientists about the gut microbiome, The Perfect Stool dives deep into the current state of research and how you can apply it to your life.
- SIBO Root Causes, Diagnosis and Treatments Episode with Dr. Nirala Jacobi, one of Australia’s leading experts in the treatment of SIBO (a common cause of IBS), is packed with information.
- Advanced Gut Testing with the Gut Goddess, Dr. Grace Liu, Episode is on bacterial overgrowths in the gut and diagnostic tests (including the OAT or Organic Acids Test). She also interprets a sample OAT test on the air and addresses restrictive diets.
- Protecting and Restoring the Gut with Naturopath Dr. Joseph Klassen Episode discusses the importance of bile and the appendix in the digestive process, the importance of butyrate in a healthy gut, the interaction between hormones and the gut, colon hydrotherapy, how to rebuild a healthy gut after antimicrobials and the reason we use herbs in food.
- DIY Fecal Transplants for Irritable Bowel Syndrome Episode is a first-hand account of someone who went this route and what you should know.
- Managing IBS with Gastroenterologist Dr Sarina Pasricha, MD by Plant Proof
In an interview with Gastroenterologist Dr. Sarina Pasricha, the topics covered in Plant Proof are how IBS is diagnosed, healing versus managing symptoms, evidence based approaches for reducing IBS symptoms, and how the Low FODMAP diet is being used incorrectly and why it is NOT Dr. Pasricha's first line of treatment for patients with IBS.
- Low FODMAP Diet and IBS Podcast
Based in Australia where so many leading researchers as well as practitioners reside, the Low FODMAP Diet and IBS Podcast covers everything you need to know about trying the diet safely and other lifestyle changes that can help manage IBS.
- Patsy Catsos RD talks about IBS symptoms and what you should know before starting a low FODMAP diet. In this episode, Larah interviews registered dietitian, Patsy Catsos, as she explains what steps need to be taken to determine if a low FODMAP diet is right for you and discusses some of the risks of following a low FODMAP if not under the supervision of a qualified dietitian.
- In the Manage Your IBS Beyond FODMAPs Episode with a registered dietitian who suffered with IBS herself shares all her insights from personal and professional experience to help others better manage IBS, why the low FODMAP diet is not for life, why it’s important to reintroduce FODMAPs into your diet to identify triggers, and what should you do if you’ve been following the diet for too long and you are scared about reintroducing high FODMAP food.
- As the prevalence of IBS is increasing around the world, the Help Non-English Speaking IBS Sufferers Episode talks about Facebook groups in different languages to help people with IBS understand the low FODMAP diet and provides other resources.
- The Gut Loving Podcast: All about IBS and the low FODMAP diet
On The Gut Loving Podcast, a dietitian and patient discuss the basics of IBS, treatment, stress, travel, food, and more.
- The F Word dives into fiber, why we need it, how to modify your intake according to your IBS-subtype and what types of fiber to avoid to prevent gas and bloating.
- Prebiotics, gut bacteria and a rainbow microbiome covers the latest science making it very easy for non-practitioners and patients to understand.
- Talking Gut with Dr. Jim Kantidakis
Talking Gut with Dr. Jim Kantidakis explores the mind-gut connection through clinical psychology, or psychogastroenterology, for both patients and health providers on everything from gut-directed hypnotherapy, cognitive behavioral therapy and others for IBS.
Documentaries and videos to watch
- The Surprisingly Charming Science of Your Gut - TEDx Talk
Scientist and author of Gut: The Inside Story of Our Body's Most Underrated Organ, Giulia Enders, teaches the funny, relatable truth about how the digestive system works, why pooping is a connection point to our mental health and the latest science on the microbiome. Get comfy, this 14-minute video is worth watching.
- The Gut: Our Second Brain on Amazon Prime
Based on research from Columbia University’s Michael Gershin, the Leonardo DaVinci of the gut, this documentary explores the power of the neurons and trillions of bacteria in our gut. The same size as a dog’s brain, by all accounts an intelligent animal, our gut behaves as a second, intelligent brain whose bacteria impacts our personalities. This documentary explores the connection between the degeneration of intestinal neurons and diseases of the gut-brain axis, like IBS or Parkinson’s. 133. Food As Medicine on Amazon Prime
Food As Medicine is a documentary that follows the growing movement of using food to heal chronic illness and disease from interviews with the field’s leading dietitians and gastroenterologists.
- The Gut Movie on Amazon Prime
Produced in 2018, The Gut Movie follows the journey of journalist and researcher Kale Brock as in the quest to discover whether the 'optimal microbiome' actually exists. He travels from Australia to Namibia to live with The San, an ancient hunter-gatherer people living traditionally from the land. Brock monitors his own microbiome and how it changes in conjunction with the new surroundings.
- Gut Reaction
Reported by ABC Science and Dr. Graham Phillips, the Gut Reaction documentary shows how the key to disease prevention may lie in how we nourish the beneficial bacteria that reside in our intestines. This "good" bacteria regulates our immune system and determines acts as the most important line of defense against harmful bacteria from the outside world. As a result, it also maintains a crucial role in mental and physical wellness.
- Explained, the Mind on Netflix
This 2019, 5-part series narrated by Oscar winner Emma Stone explores what’s happening inside the brain from dreaming to anxiety disorders.
- Ask the Doctor “The Gut Episode” on Netflix
After testing two different diets, Dr. Shalin Naik, Dr. Renee Lim and Dr. Sandro Demaio explain in The Gut Episode which foods help gut health and the latest, surprisingly effective treatments for intestinal disease.
“There are more bacteria in your body than there are in the galaxy.”
- Designer Sh*t – Coming Soon to a Theater Near You
Designer Sht is a documentary taking the audience through the filmmaker’s personal journey of research and a fecal transplant to put her colitis into remission. Hear her talk about it on The Perfect Stool Podcast.*
IBS trends around the world
- About 10 to 15% of people in the developed world are believed to be affected by IBS.
The countries where IBS is most prevalent are the United States, Peru, Brazil, Russia, and Pakistan.
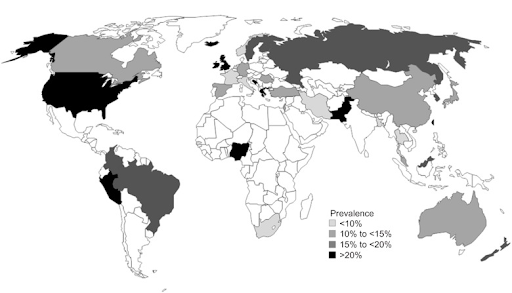
- It is estimated that 45% of people globally are affected by IBS.
- Societies with lower manual labor have more cases of IBS.
Some researchers consider this may be due to the higher level of stress perceived by people working in professional and managerial roles in industrialized societies. As a result, IBS is now being reported in Asia, South America, and Africa where urbanization is occurring rapidly.
In a nutshell
Irritable Bowel Syndrome is a complex condition. What we do know is it’s a condition based in the microbiome and can be managed with care and practice. It takes time and patience to figure out what will help you feel your best; however, healthy dietary and lifestyle changes can go a long way to reducing your symptoms and making your IBS more manageable. In fact, your best course of action likely includes a healthy combination of some of the treatments listed above.
Understanding what is “healthy” for you though can be tough, especially if you’re dealing with more than one condition alongside IBS, which is why we’re here at WeTheTrillions to help eliminate any second guessing. With the help of clinicians, we make and deliver delicious customized meals you can build healthy habits around—including ways to ease the side effects of IBS.
Simply put, we provide the insight, food, and customer service to help encourage a healthier lifestyle.
Want to learn more about how dietary changes can help ease your IBS symptoms? Start by taking our three-minute assessment.